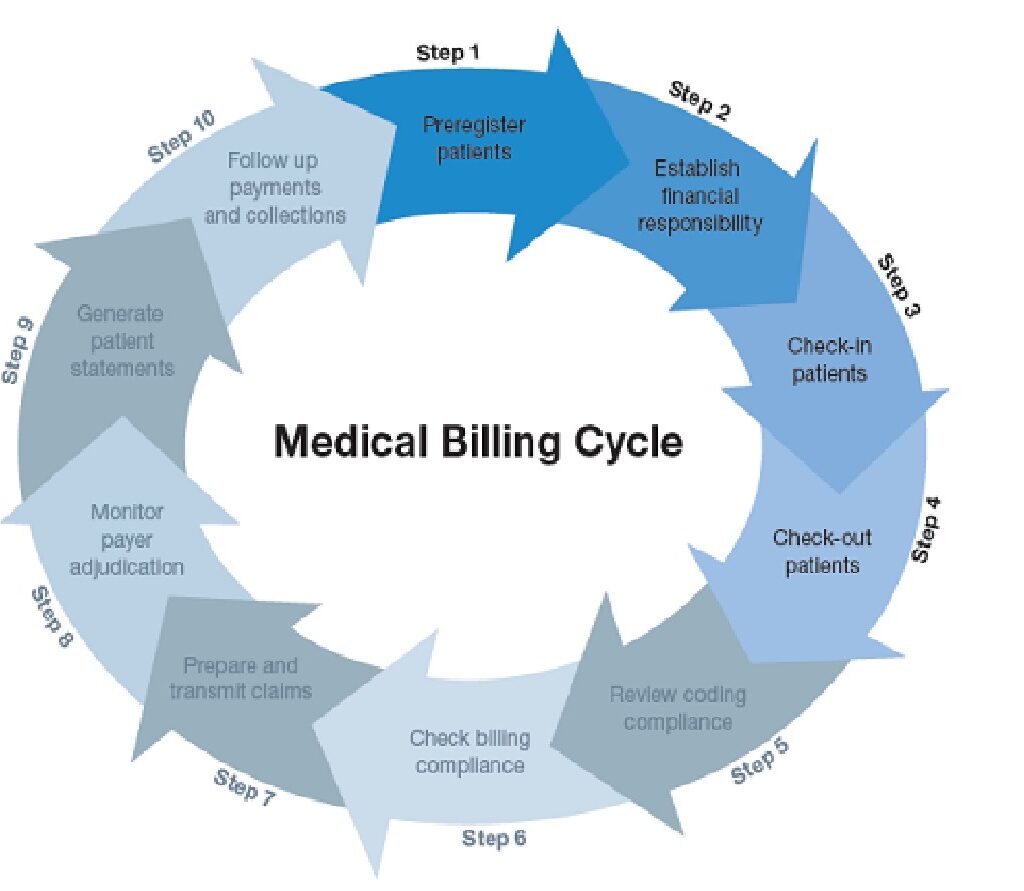
The second step in the process is to determine financial responsibility for the visit. This means looking over the patient’s insurance details to find out which procedures and services to be rendered during the visit are covered. If there are procedures or services that will not be covered, the patient is made aware that they will be financially responsible for those costs.
During check-in, the patient will be asked to complete forms for their file, or if it is a return visit, confirm or update information already on file. Identification will be requested, as well as a valid insurance card, and co-payments will be collected. Once the patient checks out, medical reports from the visit are translated into diagnosis and procedure codes by a medical coder. Then, a report called a “superbill” may be compiled from all the information gathered thus far. It will include provider and clinician information, the patient’s demographic information and medical history, information on the procedures and services performed, and the applicable diagnosis and procedure codes.
The medical biller will then use the superbill to prepare a medical claim to be submitted to the patient’s insurance company. Once the claim is created, the biller must go over it carefully to confirm that it meets payer and HIPPA compliance standards, including standards for medical coding and format.
Once the claim has been checked for accuracy and compliance, submission is the next step. In most cases, the claim will be electronically transmitted to a clearinghouse, which is a third-party company that acts as a liaison between healthcare providers and health insurers. The exception to this rule are high-volume payers, such as Medicaid, who will accept claims directly from healthcare providers.
Adjudication is the process by which payers evaluate medical claims and determine whether they are valid and compliant, and if so, the amount of reimbursement the provider will receive. During this process, the claim may be accepted, rejected or denied. An accepted claim will be paid according to the insurers agreements with the provider. A rejected claim is one that has errors that must be corrected and the claim resubmitted. A denied claim is one that the payer refuses to reimburse.
Once the claim has been processed, the patient is billed for any outstanding charges. The statement generally includes a detailed list of the procedures and services provided, their costs, the amount paid by insurance and the amount due from the patient.
The last step in the medical billing process is to make sure bills are paid. Medical billers must follow up with patients whose bills are delinquent, and, when necessary, send accounts to collection agencies.