What is Medical Coding?
Medical coding is the transformation of healthcare diagnosis, procedures, medical services, and equipment into universal medical alphanumeric codes. The diagnoses and procedure codes are taken from medical record documentation, such as transcription of physician’s notes, laboratory and radiologic results, etc. Medical coding professionals help ensure the codes are applied correctly during the medical billing process, which includes abstracting the information from documentation, assigning the appropriate codes, and creating a claim to be paid by insurance carriers.
Medical coding happens every time you see a healthcare provider. The healthcare provider reviews your complaint and medical history, makes an expert assessment of what’s wrong and how to treat you, and documents your visit. That documentation is not only the patient’s ongoing record, it’s how the healthcare provider gets paid.
Medical coders translate documentation into standardized codes that tell payers the following:
- Patient's diagnosis
- Medical necessity for treatments, services, or supplies the patient received
- Treatments, services, and supplies provided to the patient
- Any unusual circumstances or medical condition that affected those treatments and services
Why Medical Coding is needed?
Medical coding requires a particular discipline. Medical coders are considered part of the medical team, often working very closely with providers, management, and payers. A scholar, detective, educator, and problem solver, medical coders possess particular skills.
The medical coder and biller process a variety of services and claims on a daily basis. Medical codes must tell the whole story of the patient’s encounter with the physician and must be as specific as possible in capturing reimbursement for rendered services. To better understand what a coding transaction looks like, read the article: What does a medical coder do?
The main task of a medical coder is to review clinical statements and assign standard codes using CPT®, ICD-10-CM, and HCPCS Level II classification systems. Medical billers, on the other hand, process and follow up on claims sent to health insurance companies for reimbursement of services rendered by a healthcare provider.
NDC (National Drug Codes)
The Federal Drug Administration’s (FDA) code set is used to track and report all packages of drugs. The 10-13 alphanumeric character smart codes allow providers, suppliers, and federal agencies to identify drugs prescribed, sold, and used.
Modifiers
CPT® and HCPCS Level II codes use hundreds of alphanumeric two-character modifier codes to add clarity. They may indicate the status of the patient, the part of the body on which a service is being performed, a payment instruction, an occurrence that changed the service the code describes, or a quality element.
MS-DRG and APC
Two federal code sets used to facilitate payment deriving from those above systems are MS-DRG and APCs. They rely on existing codes sets but indicate the resources consumed by the facility to perform the service.
MS-DRG (Medical Severity Diagnosis Related Groups)
MS-DRGs are reported by a hospital to be reimbursed for a patient’s stay. The MS-DRG is based on the ICD-10-CM and ICD-10-PCS codes reported. They are defined by a particular set of patient attributes which include principal diagnosis, specific secondary diagnoses, procedures, sex, and discharge status. The Centers for Medicare & Medicaid Services (CMS) work with 3M HIS to maintain this data set.
APC (Ambulatory Payment Categories)
APCs are maintained by the Centers for Medicare & Medicaid Services (CMS) to support the Hospital Outpatient Prospective Payment System (OPPS). Some outpatient services in a hospital, such as minor surgery and other treatments, are reimbursed through this system.
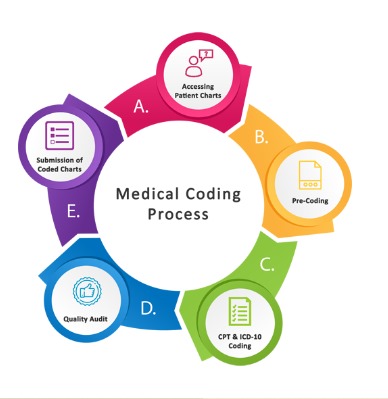
How is medical coding done?

Medical Coding is best performed by trained and Certified medical coders
A medical coder usually begins the workday by reviewing the previous day’s batch of patient notes for evaluation and coding. The type of records and notes depends on the clinical setting (outpatient or facility) and may require a certain degree of specialization (Healthcare systems may have individuals who focus on medical specialties while coders who work in smaller, or more general offices, may have a broad range of patients and medical conditions.).
Selecting the top patient note or billing sheet on the stack, the coder begins reviewing the documentation to understand the patient’s diagnoses assigned and procedures performed during their visit. Coders also abstract other key information from the documentation, including physician names, dates of procedures, and other information.
Coders rely on ICD-10 and CPT® code books to begin translating the physician’s notes into useful medical codes. An example of basic procedure documentation and subsequently assigned codes can be seen below.
How do you become a medical coder?
Successful medical coders know anatomy, physiology, medical procedures, and payer rules and policies. To become a medical coder, you must attend training via a coding-specific training program. Afterward, finding a job in the field is easier if you have a professional credential, such as AAPC’s.
There are several medical coding certifications available, depending on the area of the revenue cycle you wish to pursue. The baseline for most is the Certified Professional Coder (CPC) , which certifies the coder’s ability to work in outpatient settings. Facility coders should pursue the Certified Inpatient Coder (CIC) for inpatient coding and Certified Outpatient Coder (COC) for hospital patients receiving in-and-out services.
How much does a medical coder make in a year?
AAPC-certified medical coders make $60,917 per year on average — 29% more than uncertified health information technicians who earn approximately $47,200 annually. Where you live, what role you play in the revenue cycle, and how much education and credentials you have can influence your pay.
Charting your career requires curiosity, continuing education, and imagination. Achieving the credential is the beginning of a lifetime of new experiences and knowledge.

